
In early November, Optum Health announced it would close nearly 90 medical offices across New Jersey within weeks.
Patients received emails starting November 3, informing them that clinics would be closed from November 30 to December 5.
Most families had about 30 days to find new doctors. Some learned during office visits that their care would come to an end.
For New Jersey, this represented an unprecedented disruption to the healthcare system.
A Corporate Healthcare Behemoth

UnitedHealth Group is America’s largest health insurance and services company. In Q3 2025 alone, it earned over $113 billion.
Its insurance arm serves 50.1 million members. Optum, its clinical division, runs medical practices and employs over 90,000 physicians nationwide, making it one of America’s largest healthcare employers.
When Optum acts, millions of patients are affected.
The “Value-Based Care” Rationale

UnitedHealth is shifting to value-based care—paying doctors for keeping patients healthy, rather than paying per visit or procedure.
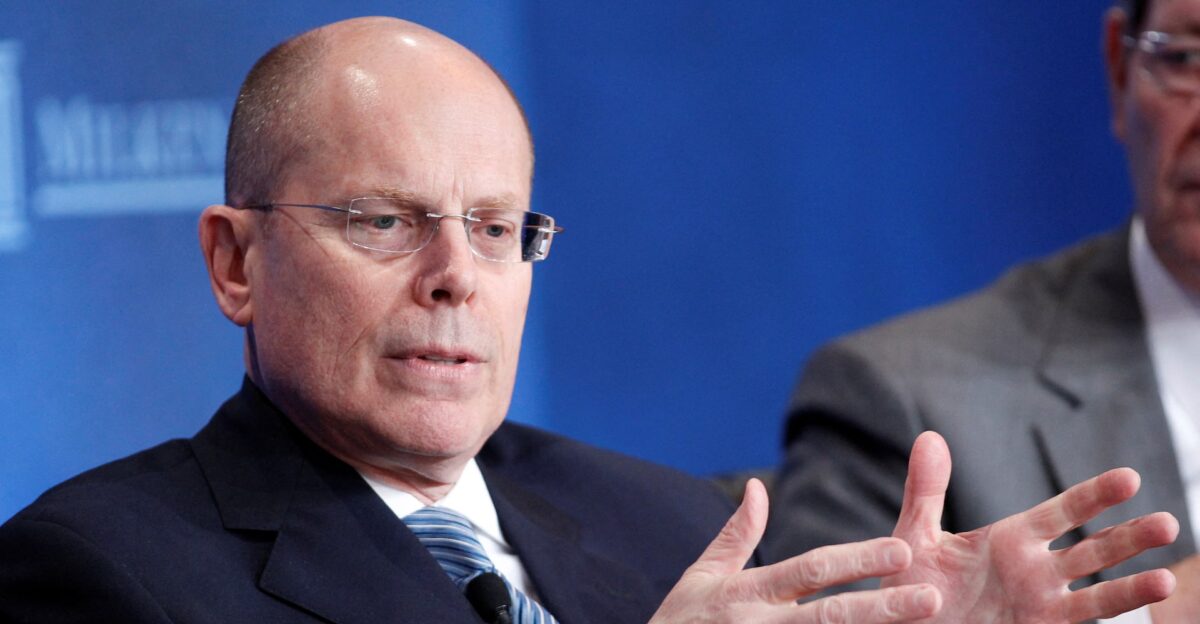
CEO Stephen Hemsley said the company regularly reviews its services and staffing.
In plain terms, Optum wanted to close clinics it considered unprofitable under this new payment model. The company framed closures as part of a strategic transformation.
The Broader Consolidation Trend

Healthcare consolidation has accelerated since 2020. Private equity made 140 healthcare deals in Q1 2025, up from 128 in Q4 2024.
Major companies, such as CVS, Walmart, and Amazon, have aggressively acquired clinics.
By 2024, 78 percent of U.S. doctors worked for hospitals or corporations, not independently. Optum alone is linked to 10 percent of all U.S. physicians.
The Scale of the Shutdown

Optum will close 90 medical offices across six New Jersey counties by late November or early December.
Closures include pediatric practices, primary care, nine gastroenterology offices, and all behavioral health services.
The company will lay off 572 employees: 390 from Optum Care, 122 from Medical Care, 49 from Services, and 11 from management.
This is one of the largest sudden clinic closures in U.S. history.
Patients Thrown Into Disarray

Niki Westra and her 10-year-old daughter Sutton went to their pediatrician’s office in Hoboken to collect medical records.
The office was closing. Sutton had seen the same doctor since infancy. “We’ve created a bond,” Sutton said.
The family now faces the reality of most New Jersey families: no referral, no continuity plan, and a healthcare market where finding good doctors is extremely challenging.
Behavioral Health Crisis

Optum is ending all behavioral health services in New Jersey by November 30. No more mental health, psychiatric, or addiction treatment.
Patients mid-treatment suddenly lose providers. Therapists lose jobs.
This timing is especially difficult: behavioral health demand has surged nationwide, and major layoffs at other behavioral health companies have already strained access to mental health care across the country.
Winter Emergency Department Strain

Experts warn that clinic closures could overwhelm emergency departments this winter as cold and flu season spreads. Research shows patients without access to primary care often go to emergency rooms instead.
Thousands of Optum patients will suddenly be left without providers. New Jersey emergency rooms are already full after the pandemic.
Wait times sometimes exceed six hours and could worsen significantly in December.
Specialty Care Gaps

The closures eliminate nine gastroenterology offices, 19 pediatric clinics, 20 primary care practices, and 12 podiatry offices. Gone too: chiropractic, dermatology, orthopedic, and endocrinology services.
In rural counties like Ocean, Camden, and Morris, these offices were the primary option, aside from hospitals. Patients with ongoing conditions suddenly lose specialists.
State health officials are scrambling to arrange new care and transfer medical records before the end of the year.
The Behavioral Health Cost Crisis
UnitedHealth has disclosed that behavioral health costs have risen significantly, negatively impacting profits.
In Q3 2025, 89.9% of premiums were allocated to medical services, exceeding the industry target of 80%. CEO Hemsley stated that behavioral health is a significant cost driver.
Closing behavioral health clinics cuts costs. But patients now seek care at hospitals instead, which actually costs the system more money overall.
The Workforce Disruption

Layoffs happen in February and March 2026—months after clinic closures. Workers know they’re losing jobs but must keep working through the shutdown.
They train replacements or handle wind-down tasks. Many Optum staff worked there for years.
The company offers job placement assistance and redeployment to other roles; however, New Jersey’s healthcare job market cannot absorb 572 medical professionals all at once.
Patient Medical Records and Continuity Chaos

Optum set up a website and email for patients to request medical records prior to closure. But many patients struggle with the process.
Elderly patients often struggle with using computers. Parents with children’s records get confused.
When records transfer slowly or incompletely, new doctors lack health history—causing delays, medication errors, and repeat tests.
Some patients can’t even access closed offices to collect records in person.
Optum’s Remaining Footprint

Optum said it will keep some pediatric, primary care, cardiology, rheumatology, and urgent care locations open in New Jersey.
But it won’t say how many or where. This suggests a bare-bones network focused only on walk-in urgent care and basic primary care.
Patients in rural areas or those requiring specialist care will struggle. The strategy appears to be shifting from comprehensive care to focusing only on immediate needs.
Regulatory and Political Response

New Jersey health officials started emergency meetings after the announcement.
They worked to help patients transfer to other healthcare systems. However, no enforcement action happened. Optum’s closures were legal under labor law and business restructuring rules.
State lawmakers inquired whether the closures violated state healthcare access rules, but corporate portfolio decisions are exempt from such scrutiny. The state cannot force Optum to keep clinics open.
The Precedent Question
Does this signal a new trend? Are big healthcare companies now willing to rapidly close entire regional networks if profits don’t meet targets?
Old consolidation waves bought practices and kept them. Optum suggests a different approach: buy, integrate, and then sell off based on quarterly earnings.
If other systems adopt this approach, healthcare access becomes unstable for patients in corporate networks. The old stability from community-based systems may disappear.
Investigating Market Power and Foreclosure

A Health Affairs study found that UnitedHealthcare pays Optum doctors 17 percent more than other providers. In markets where UnitedHealth controls 25 percent or more, payments are 61 percent higher.
Researchers warned that this may signal illegal competitive behavior. Federal Trade Commission officials and state attorneys general may now investigate whether closing these clinics reflects anticompetitive conduct.
Did UnitedHealth acquire and then abandon these clinics strategically?
Value-Based Care and Market Consolidation Paradox

Value-based care was meant to improve coordination. Instead, it accelerated consolidation and rapid closures.
Value-based care requires size and financial risk-bearing, yet it allows corporations to quickly optimize portfolios for profits.
Optum’s retreat highlights that value-based care, when combined with consolidation, creates a system where patients are rapidly abandoned if profit targets aren’t met.
Other systems may follow this concerning model.
Social Media and Public Sentiment

Social media erupted with anger after the announcement. Patients posted about chronic conditions left untreated. Behavioral health patients, mid-therapy, suddenly lost their providers. Workers faced sudden job loss.
The narrative: big profitable corporations prioritize shareholders over patients. Local news amplified these stories.
Some patients questioned why such a large, profitable company would cause such disruption. Others debated whether to sue UnitedHealth or demand government action.
The Long View

New Jersey is not alone. In November 2025, UnitedHealth closed 16 clinics in Minnesota, resulting in the layoff of 572 workers.
CVS Health closed clinics in multiple states. Humana and Cigna have done the same. The pattern: buy clinics, integrate them, then close for profit optimization.
Independent and community-based practices, by contrast, tend to remain stable in the long term.
Consolidation was intended to improve healthcare through scale, but it has created instability instead.
A Healthcare System in Transition

UnitedHealth’s closure of 90 New Jersey clinics marks a turning point in healthcare consolidation.
Corporations can now abandon communities when profits don’t align, eroding the stability patients once had.
Niki Westra’s daughter can’t see her childhood doctor due to corporate profit optimization.
Should regulators require longer notice, patient help, or service mandates? Until then, profit drives healthcare access and patient welfare.