A sweeping deal to slash the price of popular obesity drugs is poised to reshape American healthcare, signaling a rare convergence of trade policy and public health strategy. Under a proposed agreement expected as early as November 2025, the U.S. government would make medications like Wegovy, Zepbound, and Mounjaro available for $149 per month—a dramatic drop from current prices that often exceed $1,000. The plan, driven by the Trump administration, leverages trade tariffs to pressure pharmaceutical giants Eli Lilly and Novo Nordisk into accepting steep discounts in exchange for tariff relief. At the same time, Medicare is preparing to pilot coverage for these drugs, potentially transforming access for millions of Americans.
Historic Shift in Drug Pricing Tactics

For decades, high prescription drug prices in the United States have been sustained by the federal government’s limited negotiating power, especially regarding Medicare, the nation’s largest healthcare payer. Previous administrations largely relied on indirect measures or accepted rising costs. The new approach marks a sharp departure: by invoking a “Most Favored Nation” policy and wielding tariffs—tools typically reserved for international trade disputes—the administration is directly confronting pharmaceutical pricing. This is the largest single-drug price reduction ever attempted by the federal government, and it signals a willingness to use economic leverage to achieve public health goals.
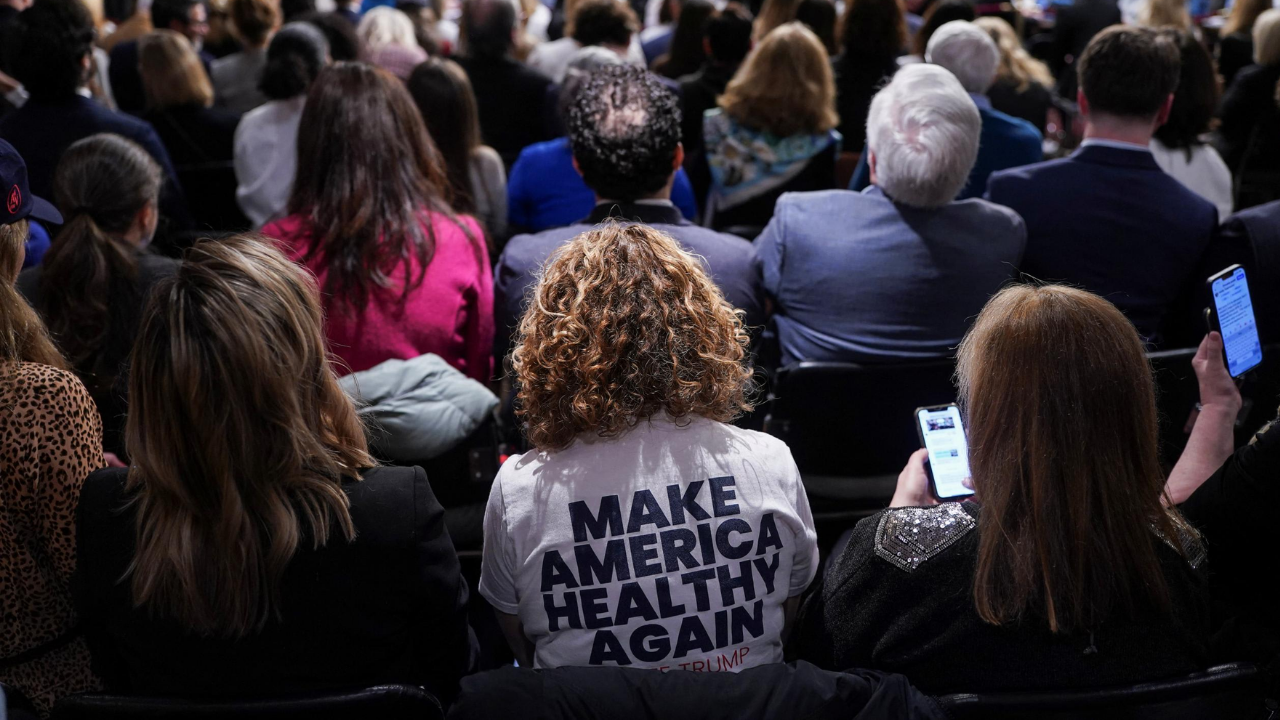
Obesity Epidemic and Demand for Treatment

The stakes are high. More than 138 million Americans, or 42% of adults, are classified as obese. The demand for effective treatments is immense, and GLP-1 receptor agonist drugs like Wegovy and Mounjaro have shown significant promise, with clinical trials reporting average weight loss of 15%. Until now, the high cost of these medications has limited their reach, especially among older adults and those on fixed incomes. By capping prices and expanding Medicare coverage, the government aims to redefine obesity as a chronic, treatable condition—potentially shifting the national conversation away from stigma and toward medical management.
Economic Impact and Industry Response

Reducing the monthly cost of obesity drugs to $149 would save individual patients between $10,000 and $12,000 annually. If 10 million Americans accessed these medications at the new rate, the collective savings could approach $120 billion each year. For Medicare, which could eventually cover up to 20 million obese beneficiaries, the financial implications are enormous. Drugmakers, meanwhile, face a new reality: lower profit margins per prescription, but the prospect of vastly increased sales volume and relief from punitive tariffs. This signals a strategic pivot from niche, high-margin pricing to a mass-market model more typical of consumer goods than specialty pharmaceuticals.
Political Dynamics and Policy Reversals
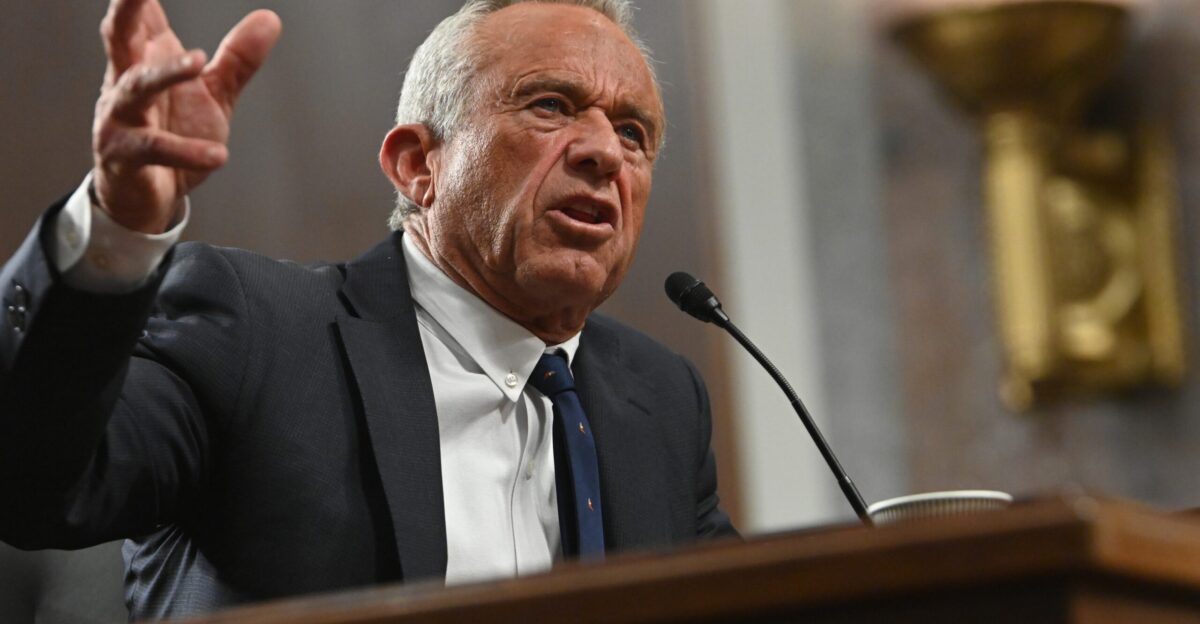
The policy shift has also exposed evolving leadership dynamics. Health Secretary Robert F. Kennedy Jr., who once criticized widespread use of obesity drugs, has reversed course to support broader access. This change reflects a pragmatic adaptation to the scale of the obesity crisis and the political momentum behind cost containment. The Trump administration’s aggressive use of trade policy stands in contrast to the Biden administration’s more cautious, incremental approach to Medicare drug expansion. The result is a volatile but potentially transformative period in U.S. healthcare governance, with alliances and strategies shifting rapidly in response to public health needs and political pressures.
Looking Ahead: Opportunities and Uncertainties
The Medicare pilot program to cap out-of-pocket costs for obesity drugs could become the largest expansion of chronic disease coverage since the introduction of Medicare Part D in 2006. However, early access may be limited by eligibility rules and pre-authorization requirements, raising questions about equity and long-term affordability. Critics warn that the $149 price point, while a breakthrough, could entrench lifelong dependence on medication and divert attention from prevention and lifestyle interventions. Internationally, the deal challenges longstanding pharmaceutical pricing structures, potentially prompting ripple effects in global negotiations. As the U.S. tests the boundaries of trade and healthcare policy, the outcome will shape not only the future of obesity treatment but also the broader debate over drug pricing and public health priorities.