
U.S. health officials report a nationwide measles outbreak in 2025 – 1,596 confirmed cases as of mid-October (the highest total since 1992).
The virus has spread to 42 jurisdictions, with Texas, New Mexico, and Oklahoma hardest hit. Experts blame recent drops in childhood MMR vaccination for opening the door, putting unvaccinated children at special risk.
Children Bear the Brunt

Almost all cases are occurring in unvaccinated people, overwhelmingly affecting children and teens. In Texas alone, there were 762 cases from late January through August, and two unvaccinated schoolchildren died of measles complications.
Nationally, CDC data show about 20% of unvaccinated measles patients require hospitalization, and up to 3 of every 1,000 infected children may die.
Outbreak After Decades of Elimination
Measles was declared eliminated in the U.S. in 2000, thanks to high vaccine coverage, but the virus has repeatedly reappeared in under-immunized communities.
The previous record year was 2019 (1,274 cases). This year’s toll has already exceeded that – over 1,500 cases, according to CDC figures – shattering the latest 30-year peak. Public health experts warn that this signals a reversal in decades of progress.
Falling Vaccination Undermines Herd Immunity

Herd immunity against measles requires roughly 95% of people to be vaccinated. But coverage has slipped below that. CDC reports 93% of U.S. kindergartners received two MMR doses in 2021–22, falling to 92.7% in 2023–24.
These small declines have left immunity gaps that measles easily exploits, especially in tight-knit communities where misinformation is common.
West Texas – Ground Zero

A single outbreak in West Texas has seeded much of the epidemic. It began in late January in Gaines County and spread into New Mexico and Oklahoma. By mid-April, 82% of the 800 U.S. cases to date were linked to that cluster.
Critically, 96% of these patients were unvaccinated or had unknown status. Three deaths have been confirmed in the cluster (two unvaccinated Texas children and one unvaccinated New Mexico adult).
Southwest States Battle the Outbreak

Texas bore the brunt: 762 cases and two pediatric fatalities by August 18. New Mexico’s outbreak (Feb–Sep) totaled about 100 cases and one death. Oklahoma and Kansas saw smaller but notable surges.
Local health agencies imposed quarantines, closed affected schools, and launched emergency MMR campaigns to stem transmission. These interventions disrupted routines but were deemed necessary to protect communities.
Heavy Toll on the Young

Two of the outbreak’s youngest victims were Texas schoolchildren (around age 8) who died of measles complications – neither had any underlying condition. By April, about 11% of all U.S. cases had required hospitalization, and roughly 1 in 5 infected young children needed inpatient care.
“We are very, very concerned about measles,” said Jessica Hancock-Allen of Minnesota’s health department, noting close work with schools and providers. The victims underscore that measles is far from benign.
Public Health Emergency Response

State and local authorities activated emergency plans. Texas DSHS rapidly set up testing and MMR vaccination clinics, launched contact tracing, and educated the public via media and schools.
The CDC issued updated guidance on patient isolation and post-exposure prophylaxis, while urging culturally tailored outreach in vaccine-hesitant communities. Together, these steps aimed to break chains of transmission and prevent secondary outbreaks.
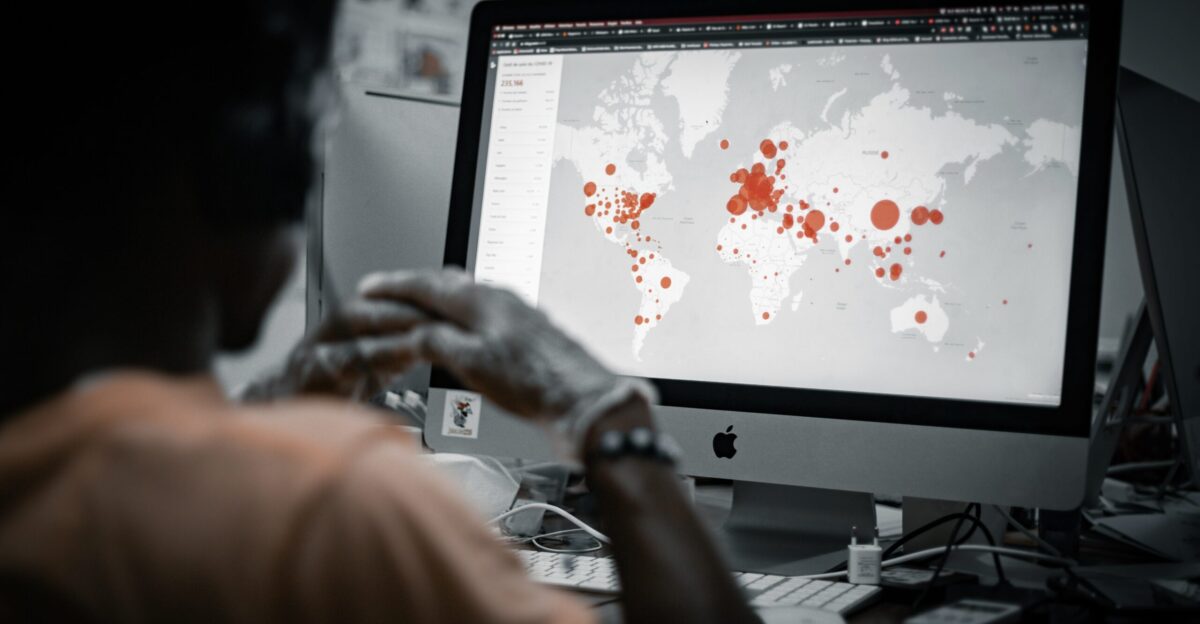
Regional and Global Trends

The U.S. outbreak is part of a wider hemispheric surge. PAHO reports over 10,000 measles cases (and 18 deaths) in ten countries of the Americas by mid-2025. Canada (4,548 cases) and Mexico (3,911) saw especially large waves.
The vast majority of those cases, like in the U.S., occurred in unvaccinated populations. “Measles is preventable with two doses… which is proven to be very safe and effective,” noted PAHO’s Dr. Daniel Salas, calling for urgent vaccination campaigns across the region.
Schools Disrupted by Quarantines

One hidden impact has been the large-scale quarantining of students after exposure. In South Carolina, more than 150 unvaccinated children across two schools were ordered to stay home for 21 days.
A Minneapolis–St. Paul’s outbreak similarly forced 118 students into quarantine. These measures – though disruptive – reflect measles’s contagiousness: as Dr. Paul Offit warned, “You have to then stay away from school for three weeks…Hundreds of children now are suffering the fact that they aren’t going to be able to go to school”.
Community Friction and Hesitancy

The outbreak has heightened tensions in some communities. In areas with low vaccine uptake, public health orders have sometimes been met with resistance or skepticism. Officials have enlisted trusted local leaders (clergy, community organizers) to encourage immunization, but rebuilding confidence remains a challenge.
Low vaccination “hot spots” continue to fuel transmission, underscoring that outreach must be sustained even as case counts fall.
Officials Push for Vaccine Confidence
Top health officials have ramped up their messaging. CDC Director Mandy Cohen has publicly stressed the MMR vaccine’s safety and efficacy, and Texas DSHS Commissioner Jennifer Shuford praised the “tireless work of public health professionals” that helped contain this outbreak.
Some states even appointed new vaccine liaisons to engage hesitant communities. The emphasis is on restoring trust: officials say high coverage and clear information are key to preventing future outbreaks.
Aggressive Vaccination Campaigns

In response, health departments are intensifying immunization efforts. Outreach teams have set up pop-up vaccination clinics in outbreak areas and schools, offering catch-up MMR doses to under-immunized families.
Thousands of residents – especially in Southwest states – have gotten vaccinated during the epidemic, nearly doubling previous year’s vaccination rates in some areas. The CDC and state agencies have also scaled up surveillance so they can rapidly detect and isolate any new cases.
Experts Warn Outbreak Could Rekindle

Even as cases have waned, experts caution against complacency. The CDC notes the U.S. resurgence reflects both domestic trends and global circulation. Modeling projections are sobering. Dr. Mujeeb Basit of UT Southwestern warned, “If vaccination rates go 5% lower, you’ll have tens of thousands of infected patients.
Rates just have to be 15% less, and you’re at millions of cases”. Without a sustained uptick in coverage, measles could regain a foothold that takes years to shake off.
Herd Immunity in Jeopardy

The key question now is whether we can rebuild the “herd immunity” that once kept measles at bay. Many school districts still hover below the critical 95% MMR coverage.
Public health officials say the coming months will test whether vaccination demand holds up – as well as the community’s willingness to re-embrace routine immunizations. The stakes are high: even a single unvaccinated cluster can spark a new flare-up.
Backlash and Policy Debates
The outbreak has reignited debate over vaccine mandates. Some state legislatures are moving to tighten school-entry requirements and limit non-medical exemptions, aiming to close loopholes that critics say allowed this surge.
Others oppose mandates on personal liberty grounds. These discussions reflect a broader conflict between individual choice and collective safety, now playing out in capitols and courtrooms.
Cross-Border Coordination

Measles doesn’t respect borders, and neither can our response. Frequent travel among communities in the U.S., Canada, and Mexico (especially religious and cultural groups with international ties) facilitated the virus’s spread. Health agencies in all three countries are coordinating alerts and sharing data.
This regional outbreak highlights the need for international vigilance – from airport screening to shared vaccination initiatives – even as countries handle their own spikes.
Legal and Ethical Tensions

The crisis raises tough legal questions. Courts may soon weigh challenges to quarantine orders and vaccine requirements, balancing public health authority against civil liberties. Ethicists note that protecting vulnerable children could justify stringent measures.
The outbreak has underscored that individual decisions about vaccination carry community consequences, a principle that policymakers and judges will have to grapple with as new cases emerge.
Shifts in Vaccine Attitudes

Public perception of measles vaccination is changing. Some parents who were hesitant are now rushing to immunize their kids after witnessing the outbreak. But misinformation still circulates, and pockets of doubt remain.
Minneapolis pediatrician Stacene Maroushek observes, “We need to do a better job of promoting… what we know from scientific data, to a level that people can understand”. The social challenge is to rebuild consensus that childhood vaccines are a shared responsibility.
Why This Outbreak Matters

The 2025 measles surge is a stark reminder that hard-won public health victories can reverse if vigilance slips. It reveals the cost of complacency: even a few percentage points drop in vaccination creates risk for everyone.
Protecting community health requires sustained effort – not just during emergencies, but in strengthening routine immunizations, fighting misinformation, and maintaining trust. The lesson is clear: we can’t afford to lower our guard against a virus once thought vanquished.