South Korea experienced a 685% increase in carbapenem-resistant Enterobacterales infections over a seven-year period—from 5,717 cases in 2017 to 44,930 by December 1, 2025.
The nation experienced its fastest growth rate for CRE infections ever. Cases surged 6.1% from 2024 alone. Public health officials warn that this crisis is reshaping how doctors handle infectious diseases.
What Is CRE?

Carbapenem-resistant Enterobacterales rank among the world’s most dangerous pathogens. WHO classifies them as critical-priority resistant organisms.
CRE forms when common gut bacteria like Klebsiella pneumoniae mutate to resist carbapenems—the last-line antibiotics doctors use.
These resistant germs spread quickly in hospitals and survive standard treatments, forcing doctors to use older, more toxic drugs.
The Antibiotic Overuse Driver

South Korea ranks second globally in antibiotic use among OECD countries, with 31.8 daily doses per 1,000 people in 2023—a sharp increase from 25.7 doses the previous year.
This nearly doubles the OECD average of 18.9 doses per person. Relaxed prescribing after COVID-19 caused the spike. Doctors prescribe antibiotics for colds and minor infections far too often.
Vulnerable Populations Under Siege

The elderly suffer most. Patients aged 60 and older account for 86.3% of CRE cases, while those over 70 years old comprise more than 31,000 of the 44,930 infections.
Nursing homes and long-term care facilities become hotspots for the spread of COVID-19. Weak immune systems and multiple health conditions put seniors at high risk. Studies show patients over 70 test positive for CRE far more often.
The Facility Transmission Problem

CRE spreads through the hands of healthcare workers and contaminated equipment. Nursing homes with weak infection control become breeding grounds. Bacteria survive in sink drains and on bed rails.
Hospitals must maintain strict protocols, utilize dedicated equipment, and thoroughly clean. Many facilities lack staff to follow these standards. Once CRE starts spreading in a facility, elderly residents face repeated infections.
High Stakes: Mortality Consequences

CRE bloodstream infections kill many patients. Those with carbapenem-resistant Klebsiella pneumoniae face 42% in-hospital death rates versus 21% for normal strains. ICU patients experience higher mortality.
Standard Klebsiella kills 17.5% of patients. A 2023 review of 157 studies found 30-day death rates at 29%, with resistant cases much worse. This shows CRE demands urgent action.
The Economic Burden

CRE infections drain massive resources. Patients need longer hospital stays, intensive care, and expensive new antibiotics. Individual cases cost $29,000 to $86,000 each. South Korea spends tens of millions yearly on CRE treatment.
These costs strain healthcare systems already burdened by aging populations. Long hospitalizations divert staff and resources, turning CRE into a major economic crisis.
Treatment Options: Limited but Existent

Contrary to sensationalized reports, doctors have FDA-approved treatments for CRE. Ceftazidime-avibactam (approved 2015) was designed to fight carbapenem resistance. Meropenem-vaborbactam works similarly.
Imipenem-relebactam and cefiderocol treat resistant strains. Colistin-tigecycline combinations are effective even against highly resistant bacteria. These drugs save lives, but doctors must prescribe carefully; they carry toxicity risks, and smaller facilities often lack expertise.
Ceftazidime-Avibactam: Proven Efficacy
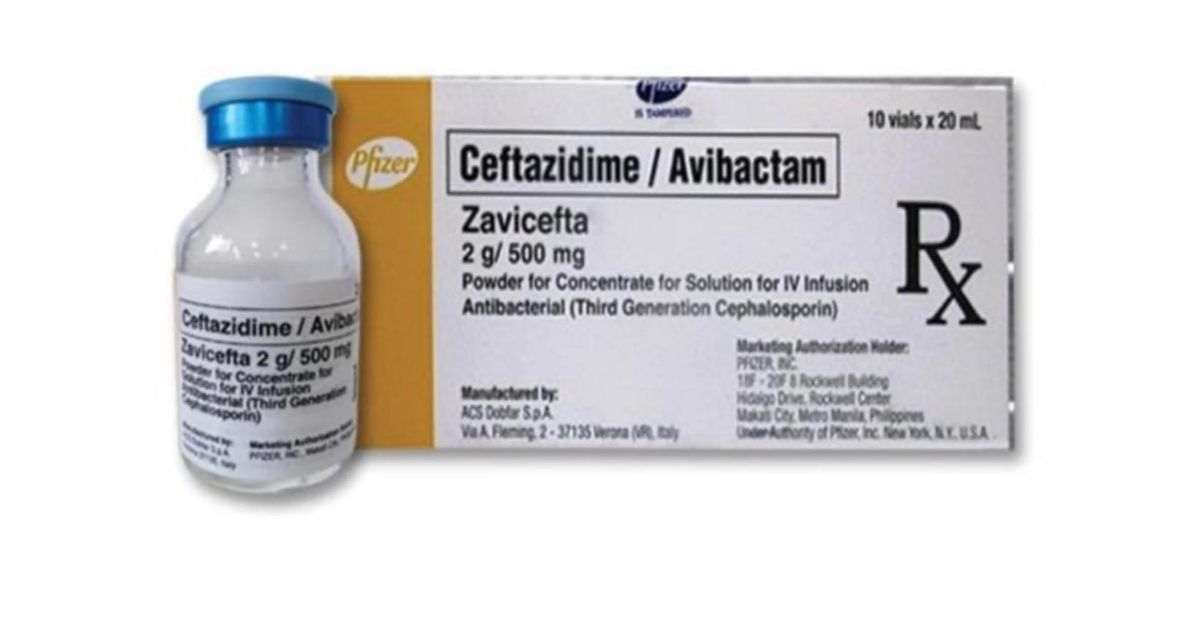
Research confirms that ceftazidime-avibactam is effective against CRE bloodstream infections. Compared to older drugs, CAZ-AVI patients experience lower 30-day death rates and higher cure rates (71% versus 35%).
Kidney damage occurs less often. Real-world cases show 60% of CRE patients respond well to meropenem-vaborbactam. Modern antibiotics achieve cure rates of 59-61%, demonstrating that these infections respond to treatment.
The Paradox: Resistant Emergence

Using newer antibiotics for CRE creates a new danger: resistance to these antibiotics emerges. Worldwide, some CRE strains are resistant to ceftazidime-avibactam and other new antibiotics. Treatment success today may create resistant bugs tomorrow if doctors don’t use antibiotics wisely.
Some new CRE variants are resistant to multiple drug types. The window to prevent total treatment failure shrinks. South Korea’s decisions now carry significant global implications.
South Korea’s Strategic Response

The Korea Disease Control and Prevention Agency finalizes its Third National Antimicrobial Resistance Plan for 2026-2030. It aims to reduce antibiotic use, preserve the effectiveness of drugs, and enhance infection control.
WHO called antimicrobial resistance a top-10 global threat in 2019. South Korea must shift from reacting to outbreaks toward planned stewardship. Success depends on strong implementation.
Antimicrobial Stewardship Programs: Early Wins

South Korea launched a pilot Antimicrobial Stewardship Program in November 2023. Trained experts review prescriptions at hospitals. Results look promising: 100% of participating hospitals used antibiotic monitoring, compared to 56.6% elsewhere.
59.2% of ASP hospitals switched to better antibiotics based on lab tests—six times higher than non-participants. These outcomes demonstrate that change is possible when resources support effective programs.
Barriers to Stewardship Expansion

Challenges block wider stewardship adoption. More than 53.6% of large hospitals lack trained specialists in antibiotics. Small hospitals and nursing homes—where CRE spreads most often cannot afford these programs.
Staff shortages prevent infection control efforts. Rural areas struggle to access training. Without serious investment in training and incentives, stewardship remains fragmented, leaving vulnerable people unprotected.
Infection Control: The Missing Link

Stopping CRE spread demands strict discipline. Healthcare workers must wear protective gear and practice good hygiene, yet many use it incorrectly.
Hospitals must clean high-touch surfaces daily and disinfect equipment between patients. Sink drains need special attention.
Most nursing homes skip these steps, allowing CRE to spread silently among residents until outbreaks force action.
The Global Threat
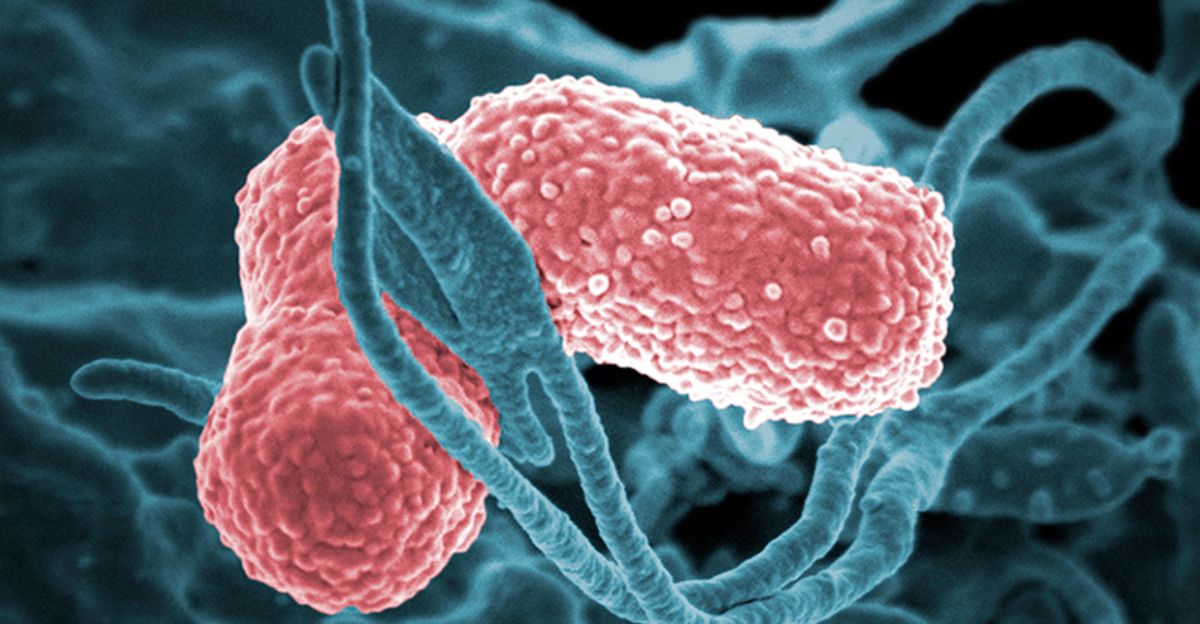
South Korea’s crisis reflects broader global trends. Klebsiella pneumoniae carbapenemase has spread globally since 1996. Carbapenem resistance continues to rise across Europe, Asia, and North America.
Antimicrobial resistance causes about 4.95 million deaths yearly worldwide, ranking with HIV and malaria. Without action, 10 million people could die annually by 2050. South Korea’s choices matter globally.
Regulatory Evolution: Tightening Controls

South Korea tightens rules on CRE. The KDCA started mandatory CRE reporting in June 2017 and expanded it nationwide by 2018. New rules limit the use of certain antibiotics in outpatient settings.
The next plan will likely demand stricter prescribing rules, require antibiotic specialists, and impose penalties for non-compliance. Twenty-five of 38 European nations already operate warning systems for resistant germs.
Supply Chain & Pharmaceutical Innovation

Global demand for new CRE antibiotics continues to rise, straining manufacturers. Companies expand production of ceftazidime-avibactam, meropenem-vaborbactam, and aztreonam-avibactam. South Korea relies heavily on imported specialty antibiotics, making the stability of its supply critical.
New drug research continues, but development costs remain high. Once-daily pills sell poorly. Makers prefer drugs for chronic conditions. South Korea may face shortages unless it stockpiles.
Public Misperception & Misinformation

Media headlines like ‘superbug crisis’ and ‘untreatable infections’ panic the public. Effective treatments exist, but they often require hospitalization and specialist care—facts that are frequently overlooked in coverage. Social media disseminates exaggerated claims based on outdated studies.
Some patients refuse hospital care, believing a cure is impossible, delaying treatment and worsening outcomes. Health authorities must communicate genuine danger without destroying hope.
Learning from Asia’s VRE Crisis
South Korea’s CRE surge mirrors the spread of vancomycin-resistant Enterococcus in the 1990s. Japan saw MRSA sweep nursing homes quickly. Thailand battled drug-resistant tuberculosis.
These cases taught us that early, aggressive response—using stewardship, improving facilities, and tracking infections—can slow or reverse resistance. South Korea knows what works. The question is whether leaders will act.
Difficult, Not Defeated

South Korea faces a serious but manageable antimicrobial resistance crisis. The 44,930 infections through December 2025 demand an urgent response. Yet data contradicts doomsday claims: proven treatments work 60-85% of the time, stewardship programs succeed, and hospitals can improve.
The real crisis is preparation gaps, not antibiotic failure. A strong response now—combining prescribing discipline, prevention, treatment access, and regulations—prevents catastrophe.
Sources:
Korea Herald, December 5, 2025
Korea Disease Control and Prevention Agency