
The U.S. Department of Health and Human Services Office of Inspector General revealed that Medicaid programs paid more than $207.5 million to health insurers for deceased enrollees between July 2021 and June 2022. The federal government’s share totaled $138.6 million.
This unprecedented nationwide audit exposed systematic failures across state Medicaid programs in verifying beneficiary eligibility and managing enrollment databases effectively.
Nearly Perfect Failure Rate

Federal auditors analyzed 100 randomly selected capitation payments and discovered 99 were improper—a staggering 99% failure rate. States had already recovered 50 payments before audit notification, demonstrating some self-correction capacity.
However, 49 payments remained unrecovered or were only addressed after federal intervention, revealing significant gaps in state oversight mechanisms and internal control systems.
Decade-Long Pattern of Waste
This isn’t an isolated incident. Since 2016, the inspector general conducted 18 separate state audits uncovering approximately $289 million in improper payments to managed care organizations for deceased enrollees.
Earlier reviews covering 2009-2019 across 14 states identified 450,562 improper capitation payments totaling $318 million, with $249 million classified as definitively unallowable under federal regulations.
How the System Works
Medicaid managed care operates through fixed monthly capitation payments. States pay managed care organizations a predetermined per-member-per-month amount for each enrolled beneficiary, regardless of actual service utilization.
When deceased individuals remain enrolled, states continue making monthly payments even though these people cannot possibly receive healthcare services, resulting in pure taxpayer waste with zero public benefit.
Privacy Laws Create Barrier

The Full Death Master File maintained by the Social Security Administration contains over 142 million death records dating to 1899. However, access remains tightly restricted under privacy laws designed to prevent identity theft and fraud.
States require special certification demonstrating legitimate fraud prevention purposes to access this database, creating significant barriers to timely death verification and enrollment updates.
Legislative Solution Enacted

President Donald Trump signed the One Big Beautiful Bill Act into law on July 4, 2025, including provisions specifically targeting this problem.
The legislation mandates that state Medicaid agencies conduct quarterly audits of beneficiary lists against the Full Death Master File beginning January 1, 2027. States must also verify provider status quarterly starting January 2028, implementing systematic death checks throughout the system.
Automated Systems Required

The new law requires states to implement automated verification processes with due process protections for incorrectly flagged individuals. States must obtain current enrollee address information and submit Social Security numbers to a new CMS system preventing Medicaid enrollment in multiple states by October 2029. These requirements represent the most comprehensive federal mandate for enrollment verification in Medicaid history.
Colorado’s Massive Problem

Colorado exemplified the crisis by making over 220,000 payments for approximately 9,000 deceased enrollees between January 2018 and December 2020.
The federal share alone totaled $3.8 million, with additional errors worth $2.2 million. State officials disputed findings and questioned Death Master File reliability, while auditors identified inadequate automated systems and insufficient internal controls as root causes.
New York Leads Losses

New York State’s Medicaid agency topped individual state losses with an estimated $23.3 million in improper payments to managed care organizations for deceased beneficiaries.
Federal authorities required the state to refund $10 million to the federal government, while managed care organizations returned $19 million. Auditors cited lack of automated verification capabilities and subpar policies as primary contributing factors.
Louisiana’s Data Gaps
Louisiana paid managed care organizations $9.6 million in per-member-per-month payments for 1,072 deceased beneficiaries.
The audit revealed median time gaps of just 23.5 days when using state vital records data, compared to 617-799 days when relying on obituaries or the Social Security Death Master File. This discrepancy highlighted critical delays in information sharing between government agencies.
Treasury Pilot Program Success

The Treasury Department demonstrated potential solutions through a five-month pilot program launched in December 2023. Using temporary Death Master File access granted by Congress, Treasury recovered $31 million in federal payments to deceased individuals.
The program achieved a 139% increase in death match detection, with projected net benefits exceeding $215 million over three years.
Bipartisan Congressional Action

Senators John Kennedy, Gary Peters, and Ron Wyden introduced the Ending Improper Payments to Deceased People Act, which the Senate passed unanimously in September 2025.
The legislation would permanently authorize Treasury Department access to the Death Master File, building on temporary three-year authorization that expires in December 2026. The bill now awaits House consideration.
Senator Scott’s Parallel Effort
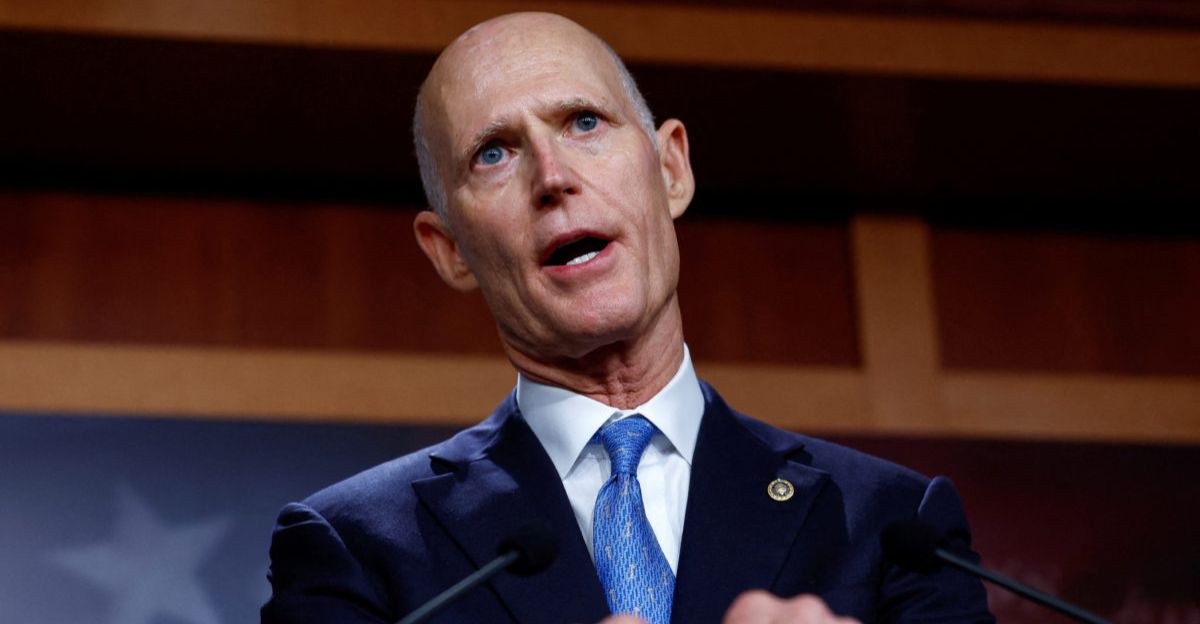
Senator Rick Scott separately introduced the LIVE Beneficiaries Act requiring state Medicaid programs to check the Death Master File quarterly to determine whether enrollees are deceased.
Scott emphasized that quarterly verification represents common-sense reform to prevent taxpayer dollars from funding healthcare coverage for people who cannot possibly use it. The bill remains under Senate Finance Committee review.
Broader Improper Payment Context

Medicaid’s deceased beneficiary problem exists within larger program integrity challenges. The Centers for Medicare & Medicaid Services reported a 5.09% improper payment rate for Medicaid in fiscal year 2024, equivalent to $31.1 billion.
Documentation issues accounted for 79.11% of these improper payments. Some independent analysts suggest actual rates exceed 25% when eligibility is comprehensively audited.
Managed Care Enrollment Trends
As of December 2024, Medicaid managed care enrollment across 29 tracked states totaled 61.7 million beneficiaries, down 3.6 million year-over-year. This 5.5% decline resulted from post-pandemic eligibility redeterminations.
National enrollment in September 2025 stood at approximately 77 million across Medicaid and CHIP, with managed care representing the predominant coverage model in most states.
Root Cause Analysis

Multiple factors contribute to persistent deceased beneficiary payments. States lack adequate automated systems for real-time death verification.
Limited Death Master File access due to privacy restrictions creates information gaps. Delays in state eligibility system updates compound the problem. Manual verification processes limit oversight capacity. Insufficient coordination between federal and state agencies allows deceased individuals to remain enrolled for extended periods.
Implementation Timeline Ahead

States face staggered compliance deadlines. Quarterly Death Master File checks for beneficiaries begin January 2027. Provider death verification starts January 2028. Multi-state enrollment prevention systems must be operational by October 2029.
Work requirements for expansion populations must be implemented before 2027. Semi-annual eligibility redeterminations for expansion adults commence January 2027, dramatically increasing state administrative workloads.
Expert Assessment

Assistant Regional Inspector General Aner Sanchez, who has investigated this issue for a decade, concluded that deceased beneficiary payments are “not unique to one state, and the issue continues to be persistent.”
The nationwide scope of the 2025 audit confirmed that improper payments represent a systemic problem rather than isolated state failures, requiring comprehensive federal intervention and standardized verification protocols.
Financial Recovery Efforts

Federal authorities continue pursuing recovery of identified improper payments. States must demonstrate enhanced internal controls and automated verification systems to prevent recurrence. Managed care organizations face increased scrutiny of enrollment data and payment reconciliation processes.
Beginning in fiscal year 2030, states exceeding 3% error rates for improper eligibility determinations will face reduced federal financial participation, creating powerful compliance incentives.
Path Forward

The combination of legislative mandates, expanded Death Master File access, automated verification systems, and financial penalties creates a comprehensive framework to address deceased beneficiary payments. Congressional oversight continues through the Senate Finance Committee.
Success depends on effective implementation of technology systems, state compliance with federal requirements, and sustained political will to maintain program integrity as administrative priority throughout changing political leadership.
Sources:
“Medicaid Agencies Made Millions in Unallowable Capitation Payments to Managed Care Organizations on Behalf of Deceased Enrollees.” U.S. Department of Health and Human Services Office of Inspector General, December 21, 2025.
“Watchdog report finds Medicaid paid more than $207 million for dead people in 1 year.” PBS NewsHour, December 23, 2025.
“Medicaid paid more than $207 million for dead people. A new law could help fix that.” Associated Press, December 23, 2025.
“‘One Big Beautiful Bill Act’: Key Final Medicaid Changes Explained.” Morgan Lewis, July 8, 2025.
“Treasury Data Pilot Prevents and Recovers $31 Million in Improper Payments.” U.S. Department of the Treasury, January 14, 2025.
“Colorado Made Capitation Payments to Managed Care Organizations After Enrollees’ Deaths.” U.S. Department of Health and Human Services Office of Inspector General, February 13, 2025.